According to the World Health Organisation (WHO), a Preterm birth is defined as a baby born alive before 37 weeks of pregnancy are completed. There are sub-categories of preterm birth, based on gestational age:
Induction or cesarean birth should not be planned before 39 completed weeks unless medically indicated.
Globally, an estimated 15 million babies are born too early every year, or in other words, preterm. That is more than 1 in 10 babies. Approximately 1 million children die each year due to complications of preterm birth. More than 60% of preterm births occur in Africa and South Asia, but preterm birth is truly a global problem. In the lower-income countries, on average, 12% of babies are born too early compared with 9% in higher-income countries. Within countries, poorer families are at higher risk.
In India, 27 million babies are born each year out of which 3.5 million babies are born prematurely as per the estimates. Preterm birth complications are the leading cause of death among children under 5 years of age, responsible for approximately 1 million deaths.
Why do premature births happen?

Why do Premature Babies need Special Care:

Various conditions might occur in premature babies. It is important for any individual who is expecting a baby soon to educate themselves with premature newborn issues.
There can be various short-term and long-term problems in newborn babies. A few of them are listed as follows:
1) Initial Breathing problems: A premature baby may have respiratory distress due to immature lungs. The lack of oxygen, as a result, can affect other organs which are immature too. This condition affects infants before 35 weeks. Infants born between 23 to 32 weeks might develop a lung disease known as bronchopulmonary dysplasia and breathing conditions known as apnea. A tube may be placed in the windpipe and a ventilator will help the baby breathe.
2) Hypothermia: A preterm baby does not have the capacity to maintain their body temperature and the ensuing hypothermia can lead to death, if not addressed. Babies are kept in a baby warmer or an incubator, with temperature control.
3) Premature babies may not be able to suckle and swallow before 34 weeks of gestation and may need a small, soft tube placed through the nose or mouth into the stomach. Sometimes very premature babies may need to be fed through the veins until they stabilize enough to receive nutrition through the stomach.
4) Heart Issues: An issue that can be serious in newborn babies is heart disease. The most common condition experienced is ductus arteriosus and low blood pressure. Babies born before 30 weeks have a high risk of developing such diseases.
5) Eyesight problems: Infants born before 30 weeks have a high risk of developing eyesight and vision problems. They may develop conditions such as retinopathy of prematurity, a condition where blood vessels swell and overgrow in the light-sensitive layer of nerves behind the eye. A premature baby may have various other conditions that can impair vision and cause blindness.
6) Hearing problems: Premature babies have the risk of developing various hearing problems. It is a must that premature babies have their hearing abilities checked before going home. It is important that premature newborn baby care is prioritized in such cases.
Due to the health risks and concerns in premature babies, they are given newborn baby care and medical attention immediately after their birth. Depending on how early the baby arrives; a neonatologist is called in to determine if the infant needs any special treatment. In addition to medical assistance, parents should seek newborn baby care tips to take care of their newborn baby.
Premature babies may have the following issues:

Treatments available in India:

The rate of premature births in India is rising and is presently around 21% of babies, according to a report released in November 2013. The report, Delivered Too Soon, was prepared by the Indian Foundation for Premature Babies (IFPB), a grouping of doctors across India. The report said three-quarters of premature babies could be saved with current, cost-effective interventions, even without the availability of neonatal intensive care facilities.
In 2012 the American Academy of Paediatrics has divided neonatal care into four distinct levels. Level I facilities (well newborn nurseries) provide a basic level of care to neonates who are low risk. They have the capability to perform neonatal resuscitation at every delivery and to evaluate and provide routine postnatal care for healthy newborn babies. Level II (specialty-level facility) is for the care of stable or moderately ill newborn babies who are born at ?32 weeks gestation or who weigh ?1500 g at birth with problems that are expected to resolve rapidly.
Level III NICUs are defined by having continuously available personnel (neonatologists, neonatal nurses, respiratory therapists) and equipment to provide life support for as long as necessary. These units have facilities for advanced respiratory support and physiologic monitoring equipment, laboratory and imaging facilities, nutrition and pharmacy support with pediatric expertise, and social services.
Level IV units include the capabilities of level III with additional capabilities and considerable experience in the care of the most complex and critically ill newborn infants and should have pediatric medical and pediatric surgical specialty consultants continuously available 24 hours a day. Level IV facilities would also include the capability for surgical repair of complex conditions.
Medical Success Stories supported by CHF:
Baby of Ancy :

The baby of Joseph and Ancy Anson was a 17-day old baby boy when the parents had contacted CHF for help. His father worked as a daily wage laborer, who lost his job due to the pandemic. His mother is a homemaker. The baby boy is the youngest child of the Ansons and has two elder siblings. Born as a preterm baby, he was suffering from neonatal seizures and sepsis. The baby was kept in the NICU and was given ventilator support for 1 week. The baby’s treatment was successfully done in Lourdes Hospital, Kerala.
The estimated cost of treatment was Rs. 3,00,000. Baby's parents were unable to gather the treatment funds, so on behalf of them, CHF raised the funds and supported his treatment.
Twins of Deevyashri :
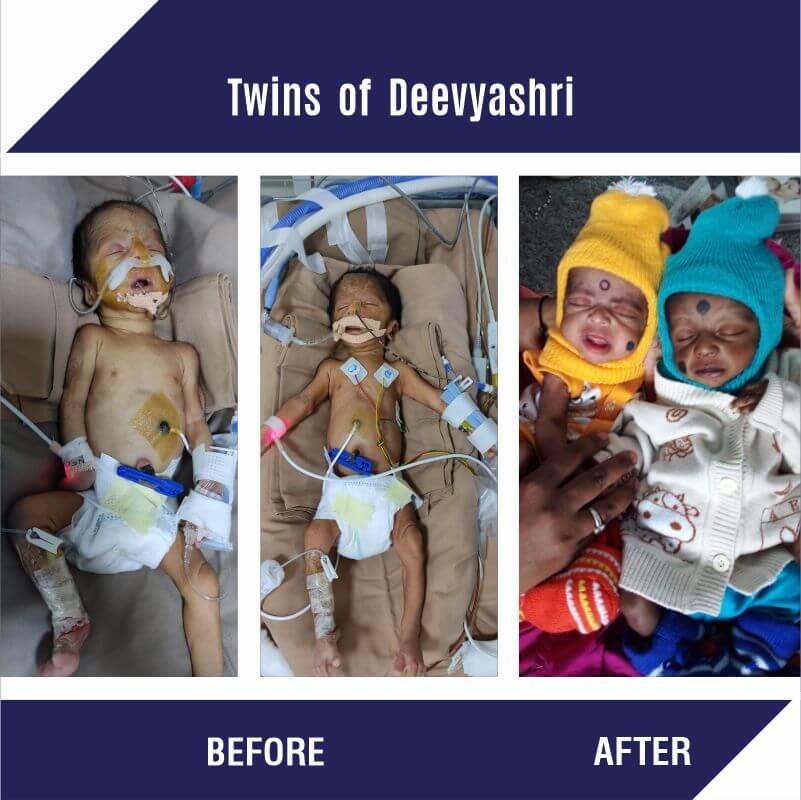
Born in the 7th month itself, the twin babies of Deevyashri and Chandrashekhar were suffering from prematurity, respiratory distress, and infections. Both the babies were kept in the NICU for their treatment. Baby 1 was given ventilator support and Baby 2 was on HFNC. Their father being the only earning member in the family with a minimum earning was not able to afford the cost of his babies' treatment and hence asked Child Help Foundation for support. After the necessary verification CHF supported the twin’s treatment.
B/O Ushakumari :

B/O Ushakumari is a 1-month-old premature baby boy from Alappuzha, Kerala. Baby’s father works as a daily wage laborer and his mother is a housewife. At birth, the baby had low weight and suffered from difficulty in breathing. He was admitted to SBM hospital, Kerala, where the doctors said that he will need CPAP and other supportive care for his breathing difficulty. The estimated cost of his treatment is Rs. 4,00,000. The family could not raise these funds due to low incomes. CHF came forward to help them by raising funds for the infant's treatment.
Since the pandemic has begun, Child Help Foundation is constantly working towards ensuring that pregnant women from underprivileged backgrounds are getting their full nutritional needs. Under our Emergency Medical Support Program, Child Help Foundation is raising funds to support the treatments of premature babies.